Revolutionizing Payer Data Integration with an AI-Driven Agent


Payer Data's Hidden Complexity
More than 1,000 payers make up the US healthcare system, and each one provides a variety of plans and data formats to meet the needs of the market. For healthcare organizations, integrating this data has become a difficult and time-consuming nightmare. Each payer provides their own formats, each with varying schemas, missing documentation, and intricate relationships across entities like claims, members, and providers.
This structural complexity creates massive inefficiencies and delays. Data teams spend weeks reverse-engineering schemas, manually validating assumptions, and writing custom pipelines for every single integration. These delays cascade through everything: quality reporting, risk stratification, operational insights, and business outcomes all get pushed back while teams wrestle with basic data formatting.
Solving the Integration Challenge with Purpose-Built AI
Gravity by Innovaccer tackles the payer integration challenge head-on. Drawing from deep healthcare expertise and hundreds of real-world payer implementations, we built a purpose-driven AI engine that transforms fragmented, undocumented payer data into clean, connected, analytics-ready datasets.
The approach eliminates dependency on manual effort or static rules. The system intelligently ingests, models, maps, transforms, and validates data, cutting integration timelines from months to days.
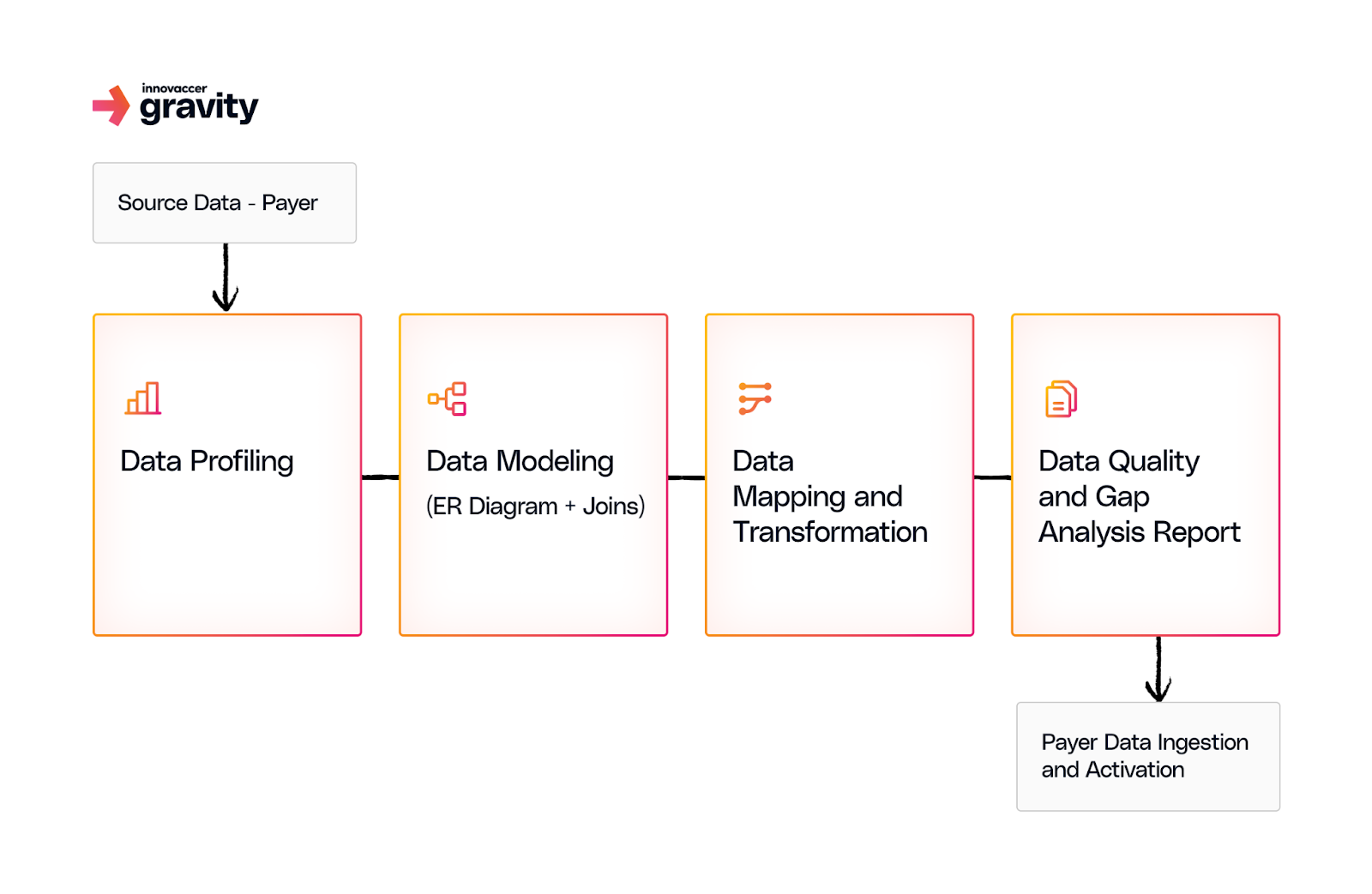
The AI-powered Data Integration Agent works through four integrated stages:
Intelligent Ingestion and Profiling: Every integration begins with the ingestion engine profiling incoming data. It analyzes schema structure, field-level distributions, sparsity, and anomalies, offering early visibility into data quality and completeness before deeper modeling begins. This proactive step eliminates blind spots that typically surface weeks into integration.
ER Mapping and Data Modeling: After profiling, the system structures data fields using statistical analysis, pattern recognition, healthcare knowledge graphs, custom-trained ML models, hierarchical clustering, and reasoning models to infer how files relate. It maps relationships between members, claims, encounters, and more, even without documentation or keys. The AI-driven modeling transforms raw files into connected datasets with accurate joins and entity relationships.
To explore how this foundational modeling works in detail, check out our blog: Solving the Hidden Crisis in Healthcare Data Integration
AI-Powered Mapping: The mapping layer is where integration often fails or drags on for weeks. The AI-powered mapping agent brings speed, intelligence, and adaptability into one seamless engine. At its core is an advanced auto-mapping system that doesn't just match field names but understands data, interprets unfamiliar schemas, infers mappings across payer variations, and dynamically adapts to new formats in real time. Key capabilities include leveraging prior integration intelligence for high-confidence mappings, applying small language models trained on payer data semantics with insights from 2,000+ integrations, and chaining prompts through RAG stores built for payer logic specificity.
AI-Driven Data Transformation: The system normalizes variations in dates, booleans and other categorical or coded fields (e.g. diagnosis codes), aligns timestamp formats and measurement units, and restructures nested or multi-column fields into analytics-friendly formats.
Data Observability
The Data Integration Agent uses Data Pulse to ensure trust in data across layers of data integration journey. Data Pulse performs hundreds of automated tests in addition to mapping and transformation, checking for completeness, accuracy, and consistency in all fields. Anomalies are caught early by these checks, and only data that passes quality standards gets integrated.
For more on how Data Pulse drives data quality, see our blog: Data Pulse - The Neural Network of Healthcare Data Observability
The Outcome
Days rather than months of payer data activation. Organizations are provided with clean, normalized data sets ready for quality metrics, reporting, insights, and downstream operational use cases without extra engineering time.
The Data Integration Agent is not only quicker, it's inherently smarter. By putting agentic workflows at each step and keeping humans in the loop, the platform ensures accuracy at scale. Every integration makes the system more clever, continuously learning to eliminate mistakes, enhance confidence scores, and speed up subsequent integrations.
Payer data integration is no longer something that takes months of specialized engineering. AI does it automatically.
Know More About Gravity by Innovaccer – Visit now

.png)





.png)









.svg)
.svg)

.svg)

